More than two thirds (69%) of health staff say they’ve experienced burnout during the pandemic, and three in five (62%) feel overwhelmed after long, intense shifts, according to a UNISON survey published today (Thursday).
As the UK confronts a surge in Omicron cases, UNISON fears many NHS staff who’ve already worked through several waves of the virus could quit, leaving the NHS in a perilous state.
The survey findings – based on responses from more than 10,000 health employees in Wales, England and Northern Ireland – show half (51%) are covering more shifts because of staff shortages. This situation is likely to worsen as NHS workers fall ill from Omicron and Delta over the coming weeks, says UNISON.
Demand on the NHS was already at unprecedented levels well before the new Covid strain, but UNISON says the pressure on staff is set to heighten even further.
Two-thirds (67%) of health employees responding to the survey say they’re concerned about the scale of the pandemic-related backlog and its impact on their workload.
More than half (57%) regularly work beyond their contracted hours. One in five (21%) do so two or three times a week, and 14% put in extra hours on every shift.
A total of (57%) of health staff surveyed are thinking of quitting their jobs. Of these, 54% say they are actively looking to leave.
The top reason given for wanting out is the negative impact work is having on employees’ mental health (67%). The feeling that their pay doesn’t reflect the jobs they do is cited by 59%, the lack of support from managers by 53%.
More than four in ten (46%) NHS staff say they feel guilty that those using health services are not getting the quality of care they need and deserve.
Four in ten (40%) health workers have had to take time off work for mental health reasons during the pandemic. A quarter (26%) sought help through their employer, but four in ten (46%) didn’t feel they got the help they needed.
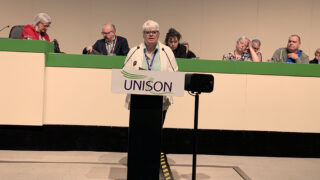
Commenting on the findings, UNISON head of health Sara Gorton said: “Staff have been wrung dry by pandemic pressures. Now they’re going through another wave as Omicron surges.
“Many are covering the shifts of poorly colleagues and feeling guilty they can’t provide quality care to patients. Overwhelmed and exhausted staff are suffering panic attacks and feeling anxious they’ll catch Covid again. It’s all taking a toll.
“The NHS was already more than 100,000 staff short before Coronavirus. The pandemic has upped the strain on health employees, and many have had enough. Poor planning by the government has made a bad situation much worse.
“The Prime Minister must minimise the staffing crisis and invest to protect the NHS. An inflation-busting wage rise paid early in the new year would be a good start. This might just be enough to persuade experienced staff to stay.”
Notes to editors: -UNISON carried out the survey from 8-29 October 2021. The findings are based on 10,602 responses from health staff in England, Wales and Northern Ireland. They were employed by the NHS (90%) and subsidiary companies, private contractors and charities working in the health service. Survey data is available on request. -Case studies (names have been changed): George, an operating department practitioner, was redeployed to an intensive care unit (ITU) during the pandemic where he was left to deal with seriously ill patients. For weeks, he had to isolate in a hotel, which affected his mental health. He says: “It felt like a war zone keeping so many patients alive. In my regular job, I’ve seen deaths, traumatic scenes and injuries. It’s grim but I don’t mind working 14-hour shifts to save lives. But ITU during the pandemic was something else. Nobody was prepared for this. After long emotionally draining days at work, I’d return to a room with no human interaction. I felt isolated, alone and got very depressed.”Lucy, a receptionist in a GP surgery, says: “We quickly got short-staffed and had to deal with an unprecedented number of calls. Often there’d be 50 patients waiting for the telephone line to open. It’s very challenging having to deal with so many people. People were understandably getting very frustrated, but the abuse was unacceptable. I’ve been called awful things, it’s very upsetting when all you’re doing is trying to help people. I’m now looking to leave the NHS for a less stressful job. It’s a shame as I love helping people and ensuring they get the care they need.” James, a paramedic practitioner says: “I’m supposed to do 37.5 hours (a week), but in reality it’s about 60. I feel constantly fatigued and the stress has taken a toll. I’ve had to take a couple of periods of sick leave to recover. Everyone is suffering burnout and staff are at breaking point. With colleagues going off sick with Omicron there are fewer of us to do the job. That means mental health teams can’t offer the expertise patients need to help them recover. I’m in two minds whether to quit or stay. Professionally I struggle with not being able to do the best for patients. But when I do make a difference, it makes me think I should carry on.” -UNISON is the UK’s largest union with more than 1.3 million members providing public services in education, local government, the NHS, police service and energy. They are employed in the public, voluntary and private sectors.
Media contacts:Liz Chinchen M: 07778 158175 E: press@unison.co.uk